Non-English Speaking Trauma Survivors (NESTS) Pathway
Background
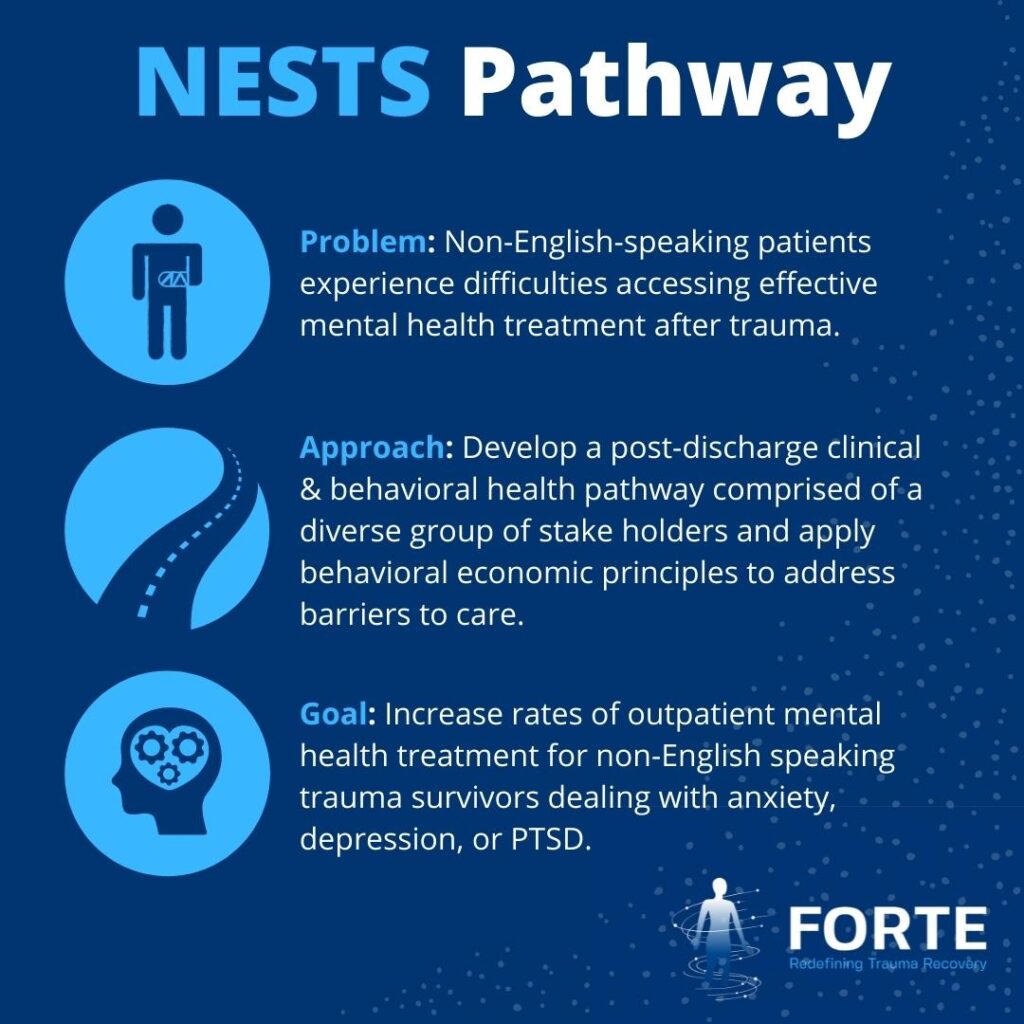
Health disparities for populations from under-represented minorities, including the Hispanic and Latinx communities, have been well documented in traumatic injuries. Among trauma survivors, non-English speaking patients are particularly vulnerable as they face cultural and language barriers that magnify the complexities of navigating the health system. Non-English-speaking patients often have difficulty finding providers with awareness and training in culturally dexterous care who speak the language in which they are comfortable communicating. As a result, compared to English-speaking trauma survivors, non-English-speaking trauma survivors are less likely to receive effective mental health evaluation and treatment, affecting their outcomes and successful reintegration into work, school, and the community.
Funded by the MGB United Against Racism initiative, this project has created a new post-discharge clinical and behavioral health pathway entitled “The NESTS Pathway.” The primary goal of this pathway is to increase the percentage of Spanish-speaking survivors of traumatic injury with a high risk of developing mental health symptoms that access a mental health evaluation and/or community-based resources to support their recovery. The NESTS Pathway employs the services of a community health worker and utilizes screening tools and technological solutions to anticipate and address systemic barriers to mental health evaluation or treatment. This project is a multidisciplinary and multi-site effort at BWH and MGH with the goal of expanding in the near future.
Findings from the Functional Outcomes and Recovery after Trauma Emergencies (FORTE) project at Brigham and Women’s Hospital (BWH), Massachusetts General Hospital (MGH), and Boston Medical Center (BMC) have shown that traumatic injury survivors experience high rates of post-traumatic stress disorder (PTSD) (15%), depression (16%), and anxiety (15%) at 6-12-months post-injury. Unpublished preliminary data from FORTE also show that among patients who screen positive for a mental health disorder at 6-12-months post-injury, Spanish-speaking patients were less likely to be receiving mental health treatment at the time of the screening compared to English-speaking patients (10% vs. 36%; p= <0.001).
Leveraging the infrastructure previously developed for the FORTE project, the team contacts, and screens for mental health conditions of all trauma survivors enrolled in the NESTS Pathway at 6- and 12-months post-injury. This project is a multidisciplinary and multi-site effort at BWH and MGH with the goal of expanding in the near future.
Initial Project Goal
Increase the percentage of Spanish-speaking trauma survivors with high risk of developing mental health symptoms that access a mental health evaluation and/or community-based resources to support their recovery from 10% to 30% by December 1, 2022.

