Improving Quality of Life for Dialysis Patients Using Machine Learning: PREDICT-AVF
Patrick V. Heindel, Mohamad A. Hussain, Wendy Williams
In new research intended to improve outcomes and quality of life for dialysis patients, CSPH research fellow Patrick Heindel, MD, along with his mentor Mohamad A. Hussain, MD, PhD, recently developed a calculator validated by high-quality, multicenter clinical data to help clinicians evaluate patients with new permanent hemodialysis access. Described in a recent article published in Nature Digital Medicine, the free online web app will help clinicians determine if and when a patient’s arteriovenous fistula (a surgical connection between an artery and vein in the arm) is ready to use for dialysis. This tool will provide a much needed enhancement to current clinical decision-making guidelines in the treatment of patients with end-stage kidney disease (ESKD), as well as potentially speeding up the often complex process of establishing a reliable hemodialysis access.
Despite high and rising rates of chronic kidney disease (CKD) in the United States, many people don’t know they have CKD until the disease is advanced and kidney failure is imminent. Over three-quarters of a million Americans live with ESKD, with most relying on dialysis to survive. The most common form of kidney replacement therapy for people with kidney failure is hemodialysis, a process by which a patient’s blood is filtered through a machine operating as an artificial kidney outside of the body. Key to making this life-saving procedure possible is the permanent vascular access,a surgically created connection between an artery and vein used to remove and return blood during hemodialysis. While the specific type of vascular access used and how much time the access point is given to mature have a great effect on a patient’s outcomes, guidelines on these topics are either often not followed or do not give clear recommendations.
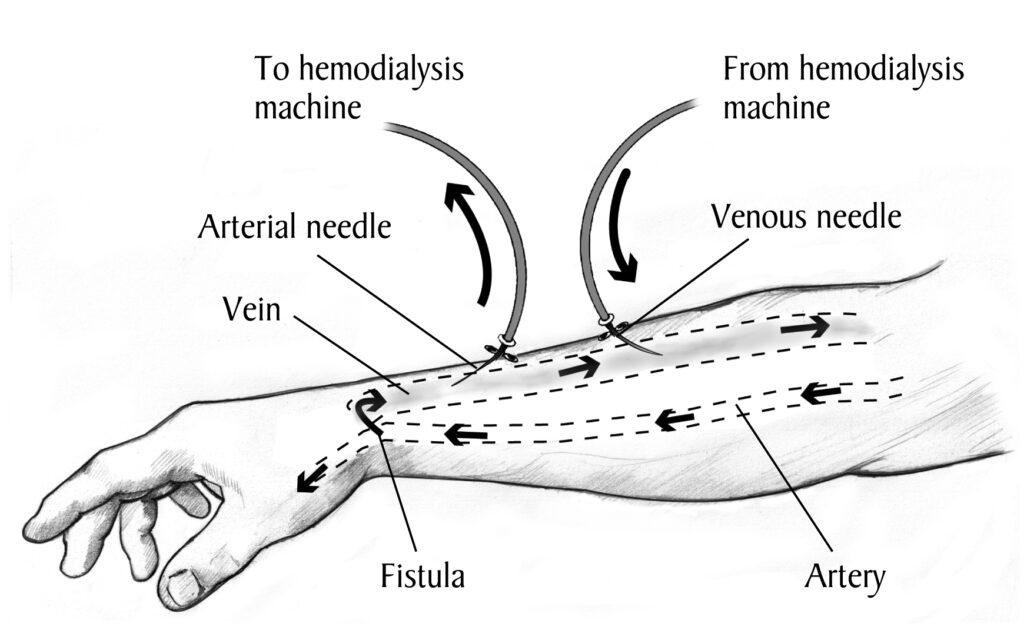
Forearm with an AV fistula and tubes inserted, with labels. Source: National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health.
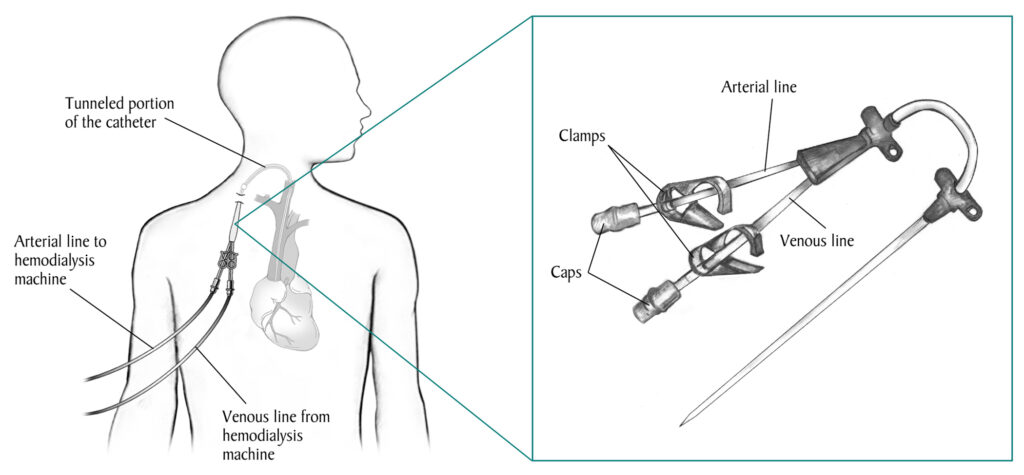
Man with a venous catheter in his neck and tubes that connect to a hemodialysis machine. Source: National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health.
For example, guidelines overwhelmingly recommend arteriovenous fistulas (AVFs) – generally created in the forearm and requiring a needle for access – over other types of access points because they provide better blood flow for dialysis, last longer, and are less likely to get infected. However, 80% of patients start hemodialysis with a central venous catheter (CVC), which uses a permanent port inserted near the collarbone. This may be due to a variety of factors, including inherent challenges in creating and maintaining a reliable AVF and delayed diagnosis of ESKD, since catheters can be used immediately, while fistulas require months to “mature.” While ESKD occurs at higher rates among Black and Hispanic patients than the general population, these patients are also less likely to receive pre-ESKD nephrology care and thus are more likely to begin dialysis with a CVC rather than a fistula.
After an AVF is created, the vein in the AVF must grow and mature over time to become robust and durable so that 1) the dialysis needles don’t damage it, and 2) it can provide high enough flows to filter all the blood. This maturation process takes time, and is different for every patient depending on their medical conditions and anatomy. Determining when a fistula is ready to use is an important clinical task. Using it too early can damage it or make it ineffective. Waiting too long can mean additional time with a CVC, which are generally used only temporarily because they can cause infections and central venous stenosis (or blood vessel narrowing) with some studies suggesting CVCs lead to accelerated death in ESKD patients.
Since figuring out how long to wait for an AVF to mature for a given patient is complicated and highly variable, Dr. Heindel and his team used machine learning to develop a web app calculator called PREDICT-AVF to help clinicians (surgeons, nephrologists, nurses, dialysis techs) better assess the maturation of a newly created radiocephalic AVF. Generally this process is highly subjective and based on experience, but for those with less experience or who want a more quantitative approach, ultrasound is the standard tool to assess the AVF maturation. Using machine learning and data from two previously conducted large multicenter prospective randomized clinical trials, the research team found that complex models with 26 clinical factors performed similarly to a much simpler model with only ultrasound flow, diameter, and the presence of a stenosis. After access creation, these anatomic variables are the only ones that seem to matter.

Patients with a low predicted probability of unassisted maturation (i.e. AVF use without any preceding procedural interventions) may need to either undergo a procedure to assist the maturation (e.g., a percutaneous balloon angioplasty) or may need to consider other access options (e.g., a graft or upper arm access). Patients with a high predicted probability of unassisted maturation may be able to go ahead and use the access and get their CVC taken out quicker. Interestingly, the PREDICT-AVF calculator performed better at predicting readiness of AVF for use than traditional static rules (such as the “rule of 6”s) that were developed many years ago based on lower quality data.
The next steps for Dr. Heindel and his team will use data from a large multicenter prospective cohort study (the Hemodialysis Fistula Maturation study) to validate the calculator and include additional access configurations (e.g. upper arm brachiocephalic access). They are additionally working on expanding this tool to predict the number and timing of interventions (e.g., angioplasties) that will be needed over the life of the access. The goal of the research team is to have the final version of the calculator included in updated society guidelines and bundled into a companion application, such as the Society for Vascular Surgery (SVS) Hemodialysis Access Clinical Practice Guidelines.


